Abstract
Introduction
Sickle cell trait (SCT) is a heterozygous condition in which individuals inherit one copy of the hemoglobin S allele (Hb S) which harbors a point mutation in codon 6 of the beta globin gene and one copy of the hemoglobin A allele (Hb A). SCT is a highly prevalent state affecting 300 million people worldwide with 5.5 million births annually. Individuals with SCT are generally asymptomatic with a normal life expectancy unlike their counterparts with sickle cell disease (Hb SS). Historically, they had been considered to have a benign condition with no adverse outcomes on quality or length of life. More recently extensive literature has been published regarding the potential morbidity associated with SCT, especially under extremes of stress or high oxygen demand states. There is a paucity of high-quality data addressing the implications of SCT on pregnancy but pregnant women with SCT appear to have an increased risk of maternal and fetal complications. We looked at the association between SCT and maternal and fetal complications via retrospective analysis.
Methods
We extracted data from the electronic medical records at our tertiary medical center on all deliveries that occurred between January 2015 and December 2020. A total of 21,198 deliveries occurred in this time frame. One hundred and sixty-two women with sickle cell trait (7.6%) were identified and matched in a 2:1 fashion to women without SCT controlling for age, gravidity, and race. Subgroup analysis by age, hemoglobin (Hb), body mass index (BMI), history of hypertension, and type-2 diabetes were carried out however subgroup analyses by a history of deep vein thrombosis or pulmonary embolism (DVT/PE) and chronic kidney disease (CKD) were not conducted due to the small frequencies in the "Yes" groups.
Results
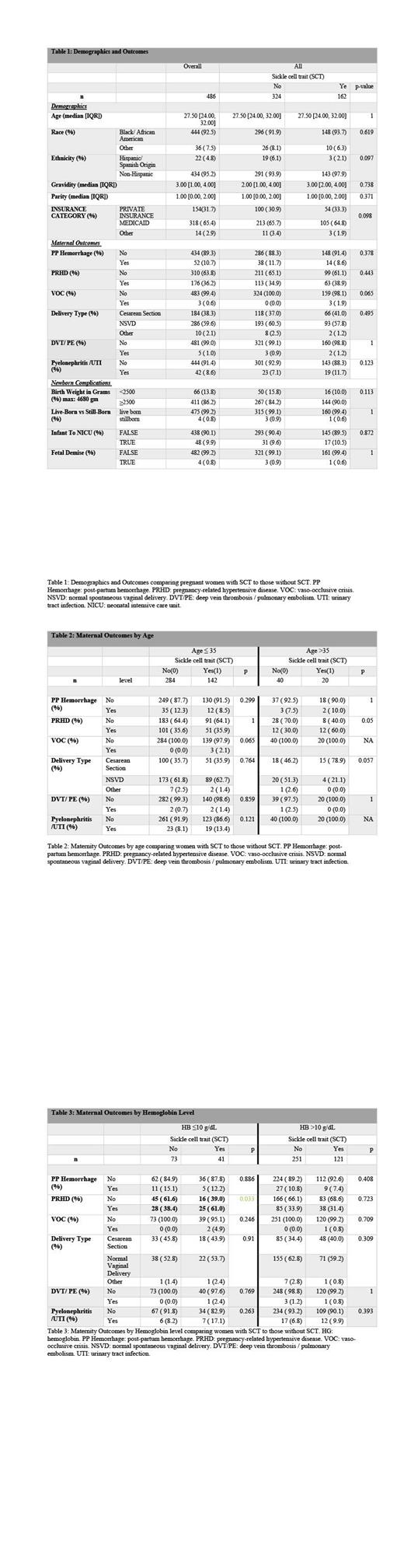
The median age was 27.5 years and 92.5% were African American. Of the cohort, 31.7% carried private insurance, 65.4% carried federal insurance (Medicaid) and 2.9% were self-pay (defined as other). Despite the lack of statistical significance between the two cohorts, some variables were noted to have numerically noticeable differences. Vaso-occlusive crisis (VOC) was seen in 1.9% of the SCT group (n=3) and in none of the control group and pyelonephritis/UTI was seen in 11.7% of the SCT group vs 7.1% in the control group (p-value 0.123) [Table 1].
On subgroup analysis by age (≤ 35 years vs >35 years) a statistically significant difference was seen in pregnancy-related hypertensive disorders (PRHD which includes gestational hypertension, preeclampsia, eclampsia, and HELLP syndrome) (60% of women with SCT vs 30% in women without SCT, p-value 0.05). VOC was only noted in women with SCT ≤ 35 years [Table 2]. When the cohorts were analyzed by Hb value ( ≤ 10 g/dL vs >10 g/dL), a statistically significant difference in PRHD was noted in women with Hb <10 g/dL (61% of in women with SCT vs 38.4% in women without SCT, p-value 0.033) [Table 3]. No differences were noted in subgroup analysis by essential hypertension, BMI, or type-2 diabetes.
Discussion
Despite the relatively small cohort, it is evident that SCT is not a benign condition in pregnancy. The racial and socioeconomic disparities are evident by the higher percentage of African Americans (92.5%) and women lacking private insurance coverage (68.3% of the cohort were covered by Medicaid or uninsured) who suffered adverse outcomes.
VOC was noted exclusively in women with SCT (0.6% of the entire cohort) consistent with the notion that stress and/or hypoxia induce sickling. The interesting findings in this cohort were related to PRHD which occurred more frequently in women with SCT older than 35 years and in women with SCT and a Hb ≤10 g/dL. Although advanced maternal age and severe anemia are known risk factors for preeclampsia, the higher incidence of PRHD in women with SCT and advanced age (>35 years) or anemia (Hb ≤10 g/dL) warrants specific examination in future studies. Additionally, studies are needed to interrogate the pathophysiology of the hypertensive disease that occurs in SCT pregnancies. One limitation of the current retrospective study is that we were unable to define the precise subtype of the PRHD. In future studies, we would specifically examine the incidence of pre-eclampsia causing PRHD in individuals with SCT.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal